
New Administrator in Little Falls Health Services


St. Francis Health Services of Morris (SFHS), is pleased to announce their Restorative Ambulation and Mobility Project (RAMP). The RAMP Project is a result of SFHS’s long term care collaborative of 7 care centers being awarded a Minnesota Nursing Facility Performance-based Incentive Payment Program (PIPP) grant by the Minnesota Department of Human Services (DHS). Implementation of the RAMP Project began January 1, 2020 and will continue through December 31, 2020.
The goal of the RAMP project is to improve the quality of care and quality of life for our residents. The project will help each resident reach their highest attainable level of function in ambulation and mobility. A Walk to Dine and a Balance Exercise program will be integrated into our Restorative Program. The Walk to Dine program will assist the resident in maintaining functional ambulation abilities to support maximum level of independence for the highest quality of life. The Balance Exercise program is intended for a resident that had a recent fall. Many respond to a fear of falling by reducing activity levels, which results in loss of muscle strength and balance. This evidence-based program would be designed and implemented to reduce fear of falling and increase activity levels.
The RAMP Project will provide us with additional resources to make positive system improvements to support good outcomes, focusing on our residents’ preferences and needs. We want our residents to experience their highest quality of life, and feel this program promotes this by impacting their ability to achieve and/or maintain their optimal physical function.
This project is another way we are carrying out our mission of “Expressing Christ’s love by providing care that values every human life.” If you have any questions about the RAMP project or want more information, please contact the care center.
Q. Why should I get vaccinated?
A. Getting vaccinated against COVID-19 is one of the best ways to protect yourself and everyone around you, particularly those who are at increased risk for severe illness. Wearing masks and social distancing help reduce your chance of being exposed to the virus or spreading it to others, but these measures are not enough. Vaccines will work with your immune system, so it is ready to fight the virus if you are exposed. Getting these shots will not only protect you from being infected; it will help us take a big step towards ending this pandemic.
Q. Why is it important for long-term care staff and residents to receive the vaccination first?
A. The average age of residents in long term care facilities is 85 and almost every one of them has an underlying health condition, and some have multiple chronic conditions. According to CDC data, the risk of mortality in this age group is 630 times higher than those 18-29 years old. While many industries can stay open or partially open with safety measures, long term care communities will not be able to return to normal until there is a vaccine.
Q. Can I visit my loved one through the window?
A. We welcome window visits, but ask that you call ahead to schedule the visit. This is to ensure we have staff available to assist your loved one to the window and provide use of an audio device if needed. Please do not open the windows during your visit to ensure the safety of our residents and staff.
We also encourage alternative means of communicating with residents such as phone calls, Facebook, Skype, etc. We have obtained additional equipment to meet the demands of these virtual visits.
Q. How will we receive the vaccine?
A. There are likely going to be two ways to receive the vaccine for your organization. Residents will receive their vaccines through the federal pharmacy partnership program (PPP). The PPP has a plan to offer multiple on-site clinics to facilitate the two doses needed for this vaccine. This infrastructure will be helpful in ensuring that long term care residents and staff are among the first to receive the vaccine.
Q. Is there are risk that I can get COVID-19 from the vaccination?
A. No, there is no risk of getting COVID-19 from the vaccination. This vaccination contains no actual COVID-19 virus. You may experience some side effects from the vaccine such as a sore arm, mild aches, or fever. This is your immune system responding to the vaccine and is expected. This does not mean you are getting sick with COVID-19. We need the vaccine to trigger this immune response to produce the immunity you need against COVID-19.
Q. How do we know it’s safe since it was developed so quickly?
A. Scientists have worked on coronavirus research for decades starting with the original SARS outbreak and influenza. Scientists only needed to isolate certain things about COVID-19 to begin creating a vaccine because we already know so much about the type of virus. Due to the public health crisis created by the pandemic, many private, government and independent groups came together and cooperated on a vaccine. This scale of cooperation is not typical, and the partnership created resources and information sharing to develop the vaccine faster.
Q. What are the side effects of the vaccine? Are there long-term effects?
A. There may be side-effects from the COVID-19 vaccination such as a sore arm, mild, generalized aches, headache, and fever. These side effects are more common after the first injection and not as common after the second injection. This vaccine will not make you sick with COVID-19; the side-effects are a result of your body’s immune system working to understand and create a response to the virus which is needed for your immunity. The long-term effects are still being studied. The first two months show no severe side effects. As with all vaccinations, long-term effects are monitored for up to 10 years.
Q. Should / can I still get a flu shot?
A. It is important you still receive a flu shot. However, it is not recommended to have a flu shot within one month of the COVID-19 vaccine. If you have not already received your flu shot, speak with your supervisor or your doctor about the best plan for receiving flu vaccine and COVID-19 vaccine.
Q. Will I have to pay for it?
A. No, there will be no cost for residents or staff for the vaccine.
Q. How many shots will I need and when?
A. The vaccine includes two injections. The second injection will either be given 21- or 28-days after the first injection. The timeframe for the second injection depends upon the manufacturer and what is written in the emergency use authorization. Your organization will make sure you have this information once vaccines are distributed and ready for administration.
Q. How long is the vaccine effective?
A. We don’t know. Because the vaccine is new, the length of immunity is unknown. There are some vaccines that do not require additional shots and there are other vaccines, such as the tetanus vaccine, that require periodic boosters. The vaccine will continue to be studied over time and if additional boosters are needed that information will be released when it is known.
Q. Is it better to get natural immunity for COVID by getting the virus instead of the vaccine?
A. In many cases, the way to develop natural immunity to a pathogen is to become sick, have our immune systems respond, and then our immune system “remembers” the pathogen to keep us from getting sick again. However, our immune systems cannot always “remember” the pathogen; or, it cannot always fight off the virus. Right now, we don’t know if becoming sick with COVID-19 actually causes you to be immune to re-infection with the virus or not. We believe the vaccination does provide immunity to the disease. Additionally, there is no way to predict whether or not someone with COVID-19 will develop severe disease and suffer significant health complications or not; becoming sick is a risk and there is no way to predict the outcome of illness. You will not become sick from the COVID-19 vaccine.
Q. What happens when long-term care residents are vaccinated? Can we begin to reopen our community?
A. Long term care facilities will not be able to return to normal until a vaccine is administered to most residents and staff. As soon as we start to successfully administer the vaccine in our communities, we hope can begin to discuss what’s next for our community and for long-term care communities across our state. Until that time, please continue your infection prevention and control practices and follow the most current visitation guidance, even after you start vaccinations.
Q. Do you have enough personal protective equipment (PPE) for residents and staff?
A. We have sufficient personal protective equipment at this time. We continue to monitor our supplies.
Q. How are you keeping residents and staff safe?
A. In addition to visitor restrictions, residents are social distancing, wearing masks when outside of their room. Any small group activities are being monitored. Staff are completing full vital signs daily on our residents. Temperature checks and respiratory assessments are repeated on a later shift.
All staff are being screened before coming into work and are required to wear face masks and eye protection in our communities. We have provided staff with additional face masks to wear while off duty.
We continue to routinely test facility staff according to CMS guidelines. “Facility Staff” is broadly defined to include employees, consultants, contractors, volunteers, and caregivers who provide care and services to residents on behalf of the facility, and students in the facility’s nurse aide training programs or from affiliated academic institutions. Our care center is in a level county positivity rate. The requirements outline routine testing depending on our county positivity rate:
We continue to follow the recommended guidance from the Centers for Disease Control & Prevention (CDC) and Centers for Medicare & Medicaid Services (CMS), and the Minnesota Department of Health (MDH), and take all appropriate measures possible to protect the health and wellness of all who live and work here. We test symptomatic residents and staff as symptoms arise and perform entire-site testing during an outbreak (1 or more positive cases of either a resident or staff in our care center). Should a confirmed case come from any of these tests, we would promptly notify our residents, their families and staff.
Q. What if a resident tests positive?
A. In the event we have a confirmed positive case on our care campus, we would notify all residents, staff, and immediate family contacts. (Please insure we have updated contact information.)
As we monitor the care centers in MN surrounding us who have experienced caring for residents testing positive for Coronavirus and a loss of staff due to the outbreak, we continue to refine our plan to manage an active case in our care center. In the event your loved one is diagnosed with COVID-19, we must transfer them to a segregated and quarantined unit to properly meet their care needs and protect other residents from further outbreak. There are many issues to consider related to maintaining the segregated unit but the greatest concern is staffing, both within and outside of the segregated unit. Our hope is that our staffing would remain constant, but care centers that have experienced an active case, see as much as a 20% loss of their nursing staff due to exposure or requested Leaves of Absence. For that reason, it may be necessary to transfer the resident who tests positive to a nearby location or affiliate care center that has the necessary equipment and staff needed to care for COVID-19 patients.
In the event we do get a confirmed case in our care center, we are prepared to complete entire site testing. Residents and family will be consulted prior to any testing.
The care center will determine exposure risk and evaluate whether or not to discontinue communal dining and small group activities based off risk. Indoor visits are restricted for 14 days after any positive case of COVID-19 in Residents or Staff.
Q. What if a staff member tests positive?
A. In the event we have a confirmed positive case on our care campus, we would notify all residents, staff, and immediate family contacts. (Please insure we have updated contact information.)
Any staff member that tests positive would not be allowed to return to work for 10 days following the positive test and 72 hours from the last fever without using medications.
In the event we do get a confirmed case in our care center, we are prepared to complete entire site testing. Residents and family will be consulted prior to any testing.
The care center will determine exposure risk and evaluate whether or not to discontinue communal dining and small group activities based off risk. Indoor visits are restricted for 14 days after any positive case of COVID-19 in Residents or Staff.
Q. How can I visit my loved one?
A. Indoor visits are available for counties in the green and yellow positivitiy rate. The care center has gone 14 days since the last confirmed case of COVID-19.
Alternative opportunities for visits by appointment include,
-Virtual visits. — We encourage alternative means of communicating with residents such as phone calls, Facebook, Skype, etc. We have obtained additional equipment to meet the demands of these virtual visits.
-Open or closed window visits with social distancing and the use of PPE.
-Outdoor patio visits with social distancing and Personal Protective Equipment (PPE) as required upon visitor successfully passing the visitor screening. All outdoor visits must be monitored by staff.
Q. Are you testing all residents and staff?
A. We continue to routinely test facility staff according to CMS guidelines. “Facility Staff” is broadly defined to include employees, consultants, contractors, volunteers, and caregivers who provide care and services to residents on behalf of the facility, and students in the facility’s nurse aide training programs or from affiliated academic institutions. Our care center is in a level county positivity rate. The requirements outline routine testing depending on our county positivity rate:
We continue to follow the recommended guidance from the Centers for Disease Control & Prevention (CDC) and Centers for Medicare & Medicaid Services (CMS), and the Minnesota Department of Health (MDH), and take all appropriate measures possible to protect the health and wellness of all who live and work here. We test symptomatic residents and staff as symptoms arise and perform entire-site testing during an outbreak (1 or more positive cases of either a resident or staff in our care center). Should a confirmed case come from any of these tests, we would promptly notify our residents, their families and staff.
Q. Are the salons resuming?
A. The salons are resuming following the guidelines set out by the MDH and CDC. Beauticians will be screened prior to entering the building. They will wear a surgical mask and perform proper hand hygiene before and after contact with a resident. Clients will enter the salon one at a time. They will be required to wear masks throughout the entire appointment. If the care campus is experiencing a COVID-19 outbreak, the care center sill suspend salons services until there are no longer residents testing positive.
Feeling stressed? Worried about COVID-19? Family struggles getting harder? Here’s a free, confidential resource to call for a 20-minute coaching session about coping with the stresses of COVID-19:
Call 612-455-8656
or
email covidsupport@acp-mn.com
This hotline is funded by a LeadingAge MN Foundation grant through the Minnesota Department of Human Services and is being offered through October 2, 2020. No caller information will be shared with our organization or the funder. It’s free, confidential, and convenient!

May 10th-16th, 2020
National Skilled Nursing Care Week has been held annually since 1967. It was created by the American Health Care Association to recognize the vital role care centers have in providing for our seniors. For years, care communities use this week to share the relationships that develop between staff and residents; the activities that are a part of each day and the memories made by all who live and work within its care communities. This event is an opportunity to display the advances in person-centered care and the achievements of the care centers. However, like most scheduled events this year, Skilled Nursing Care Week will be different. Friends and family will not be able to enter the buildings to join in the celebrations. Never the less, it is more important than ever to honor our residents and staff for the work they do within a skilled nursing care center. We urge everyone to join in virtually to support our residents and staff.
“Sharing Our Wisdom” is the 2020 theme for National Skilled Nursing Care Week. This theme intends to celebrate the residents and their staff by showing the unique insight our seniors have on life. This speaks volumes for what our world is currently enduring. Our seniors have a way of reminding us to be present, to cherish what we have and to not take things for granted.
As we start this week, we want to say thank you to all those involved in helping enrich the lives of our seniors. We appreciate all of our staff and volunteers for their incredible dedication and passion for their work. This year St Francis Health Services received the Award of Merit for Performance Excellence in Aging Services from LeadingAge Minnesota for our demonstrated commitment to quality and continuous improvement. We recognize that this would not have happened without the strength of our staff who continue to surpass any expectations we may have and bring joy to our residents every day.
We appreciate you and we thank you for every kind act that you show to those you work alongside to provide care for those entrusted to us!
-St. Francis Health Services
We at St. Francis Health Services of Morris take caring for your loved ones very seriously.
In response to coronavirus (COVID-19) we have aggressively implemented prevention and preparedness activities in all of our care centers (nursing homes, assisted livings, and group homes).
These interventions are intended to address the risk for our residents and employees from contracting and spreading the COVID-19. We continue to follow guidelines provided to us by the Centers for Disease Control and Prevention (CDC), the Centers for Medicare and Medicaid Services (CMS), and our local and state health agencies.
Visitor Restrictions:
Other Infection Control Practices:
Status of COVID-19 Monitoring:

St. Francis Health Services Recognized for Achievement in Quality Morris, MN – February 5th, 2020 – St. Francis Health Services received the Award of Merit for Performance Excellence in Aging Services from LeadingAge Minnesota for its demonstrated commitment to quality and continuous improvement. “Quality improvement in long-term services and supports is a continuous process, bettering our best each day to provide exceptional care and services to older adults,” said Gayle Kvenvold, President and CEO, LeadingAge Minnesota. “We congratulate St. Francis Health Services for their demonstrated commitment to quality in all that they do. By completing this intensive program, St. Francis Health Services and their dedicated employees are working together as a collaborative team to deliver higher quality care and services to the older adults they serve.” Performance Excellence in Aging Services was created by LeadingAge Minnesota in 2017 to help aging services providers innovate and improve the quality services and supports they provide to older adults. The continuous learning and development program is centered on the core values and criteria of the Baldrige Performance Excellence Program, which focuses on seven areas of achievement and improvement: leadership, strategy, customers, measurement, workforce, operations and results. To achieve the Award of Merit, St. Francis Health Services completed an in-depth organizational self-assessment to identify, prioritize and address improvement opportunities in their organization. By completing this initial phase of the Performance Excellence in Aging Services program, St. Francis Health Services has demonstrated that they have effective systems in place that will enable them to better serve older adults, empower staff teams, and achieve and sustain quality efforts more efficiently and effectively. Carol Raw, CEO/President states “As the newly appointed CEO/President of St. Francis Health Services, I sought confirmation from an external source that the systems we had in place were truly aligned with our strategic goals; that the services we provide are a reflection of the needs of the communities we serve and that our leadership staff are engaged in the creation of, and accountable for, the strategic plan outcomes. I also felt the messaging of our mission and core values had lost its strength as the main cultural component. While we had many quality initiatives in place, ironically we had no corporate level quality review to identify as a team the cause of our problems, or a method to create and implement action plans to resolve problems and achieve objectives. Each of these areas have now been addressed and we are beginning our first year of accountable strategic planning using annual objectives and action plans to measure our progress. The Performance Excellence program provided us with the tools to methodically assess our organization and collaboratively reach an understanding of who St. Francis Health Services is overall, but specifically in the areas of leadership, strategy, customers, measurement & analysis, workforce, operations and results. We are excited to continue down the path of assessment, but more so in working together as an executive and operational leadership team, to take meaningful strides forward in our continuous quality improvement.” For more information, contact Cami Peterson-DeVries, VICE PRESIDENT of Corporate Compliance & Ethics and Leadership Development at 320.589.4922 or cpeterson-devries@sfhs.org. About Organization St. Francis Health Services of Morris, Inc. (St. Francis) was created in 1984 as a not-for-profit organization committed to providing quality services to people of all ages with physical, mental and intellectual disabilities. Our service focus is the rural areas of MN with populations under 20k although we own and operate care centers in Duluth MN and a campus in Farmington MN. St. Francis was formed specifically to strategically expand services to meet the complex and diverse needs of vulnerable aging adults and people of all ages with physical, mental and intellectual disabilities. St. Francis’ corporate office provides operating support and oversight for 13 SNFs, 10 Assisted Living, 2 Independent Living and 74 Community Based Residential Group Homes throughout the state of Minnesota. St. Francis’ services include skilled nursing care (subacute, long-term, and memory care), assisted living with home healthcare and memory care, a full range of therapies, and community and residential services to people with physical, mental, and intellectual disabilities. St. Francis provides care to 838 residents within our SNFs, 342 tenants within our Assisted Living properties, and 309 persons who receive residential group home services in communities throughout MN. About LeadingAge Minnesota Driven to transform and enhance the experience of aging, LeadingAge Minnesota works alongside its members, caregivers, advocates and consumers to collectively shape the future of aging services and ensure older adults in every community live with dignity, meaning and purpose. Together with more than 60,000 caregivers, LeadingAge Minnesota members provide services and support to nearly 70,000 older adults every day in independent senior housing, assisted living, adult day, home care and skilled nursing settings.
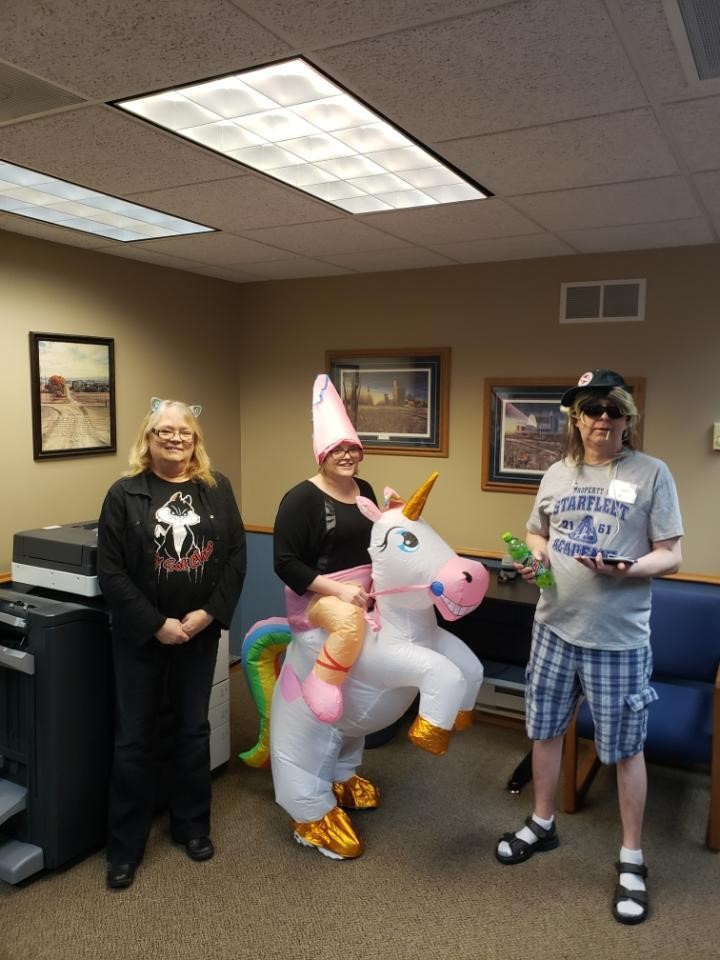
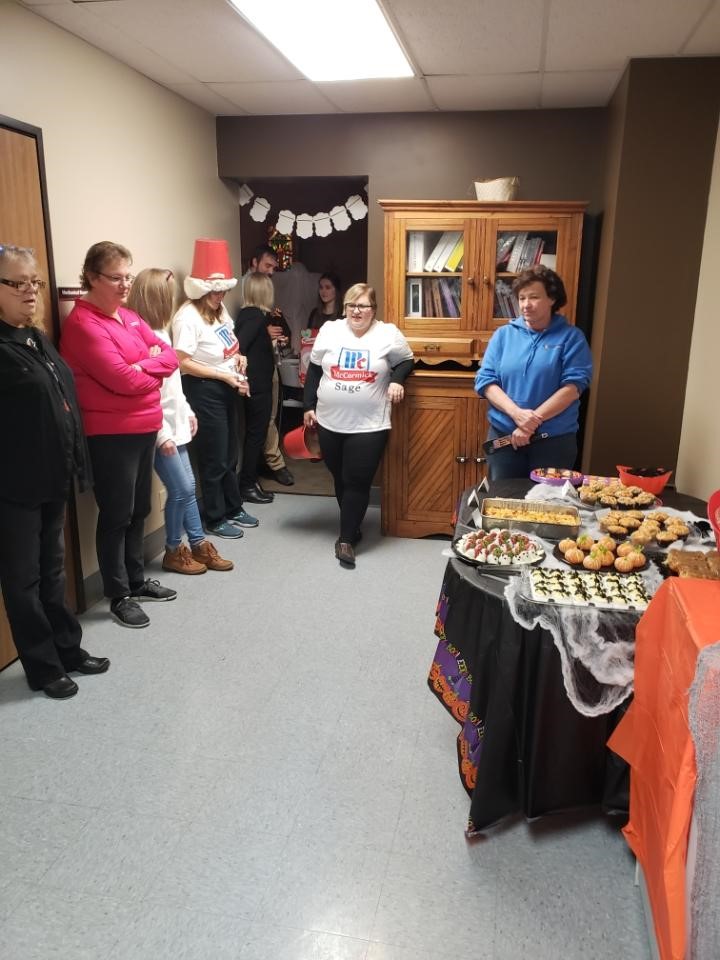
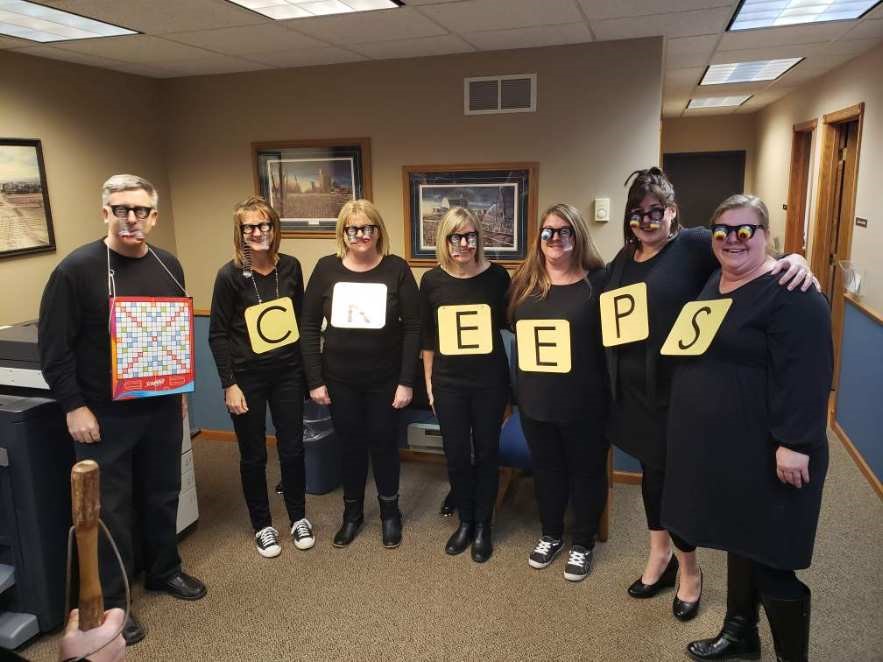
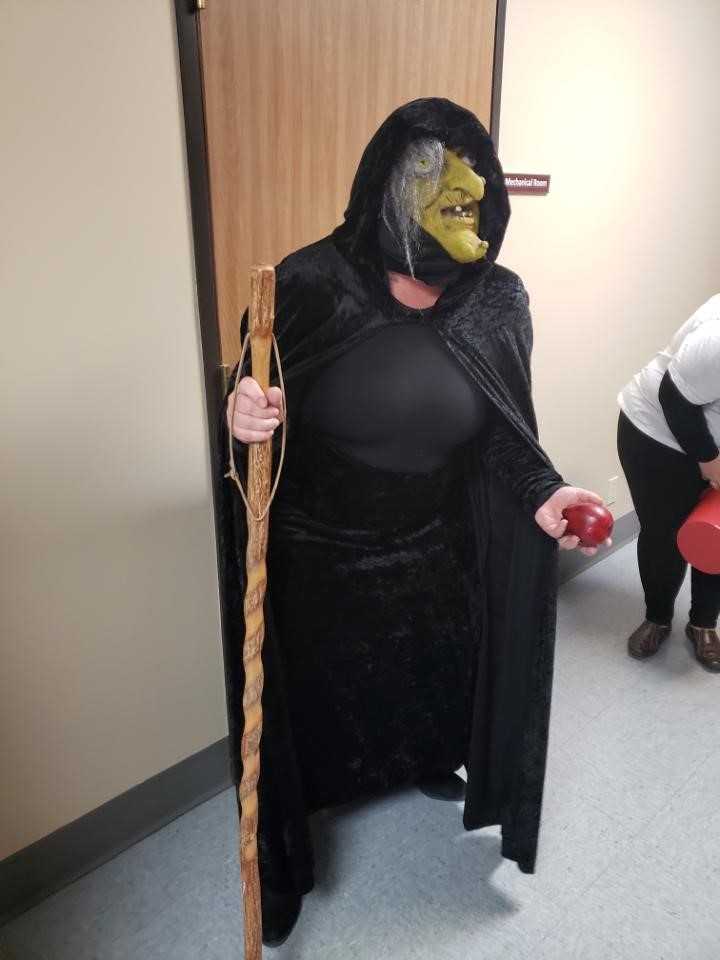
St. Francis Health Services corporate employees enjoyed some Halloween fun with a costume contest and festive Halloween goodies. Thank you all that attended the event but mostly for being part of a great team!




St. Francis Health Services of Morris recognizes our retiring Governance Board members who dedicated their valuable time and skills for the last 8 years. Thank you Steve Lienemann and Neil Schmidgall for believing in our mission and offering invaluable leadership and support. Steve continues to serve as a member of our sponsorship board